The Sechenov Medical Journal is a scientific and practical peer-reviewed journal, the official publication of Sechenov University.
The Journal has been published since 2010 with a frequency of 4 issues per year and is intended for the health professionals.
The journal is ranked at Level 1 on the Unified State List of Scientific Publications, also known as the 'White List'.
The Title is included in the Russian Science Citation Index (RSCI) collection, based on the Russian Index of Science Citation(RISC) database and is in the Scopus database.
Sechenov Medical Journal publishes original articles, reviews, and clinical cases, covering a wide range of issues in biomedical sciences, fundamental and clinical medicine and concerned with important clinical and basic research in the field of:
- cell biology,
- pathological physiology,
- internal diseases,
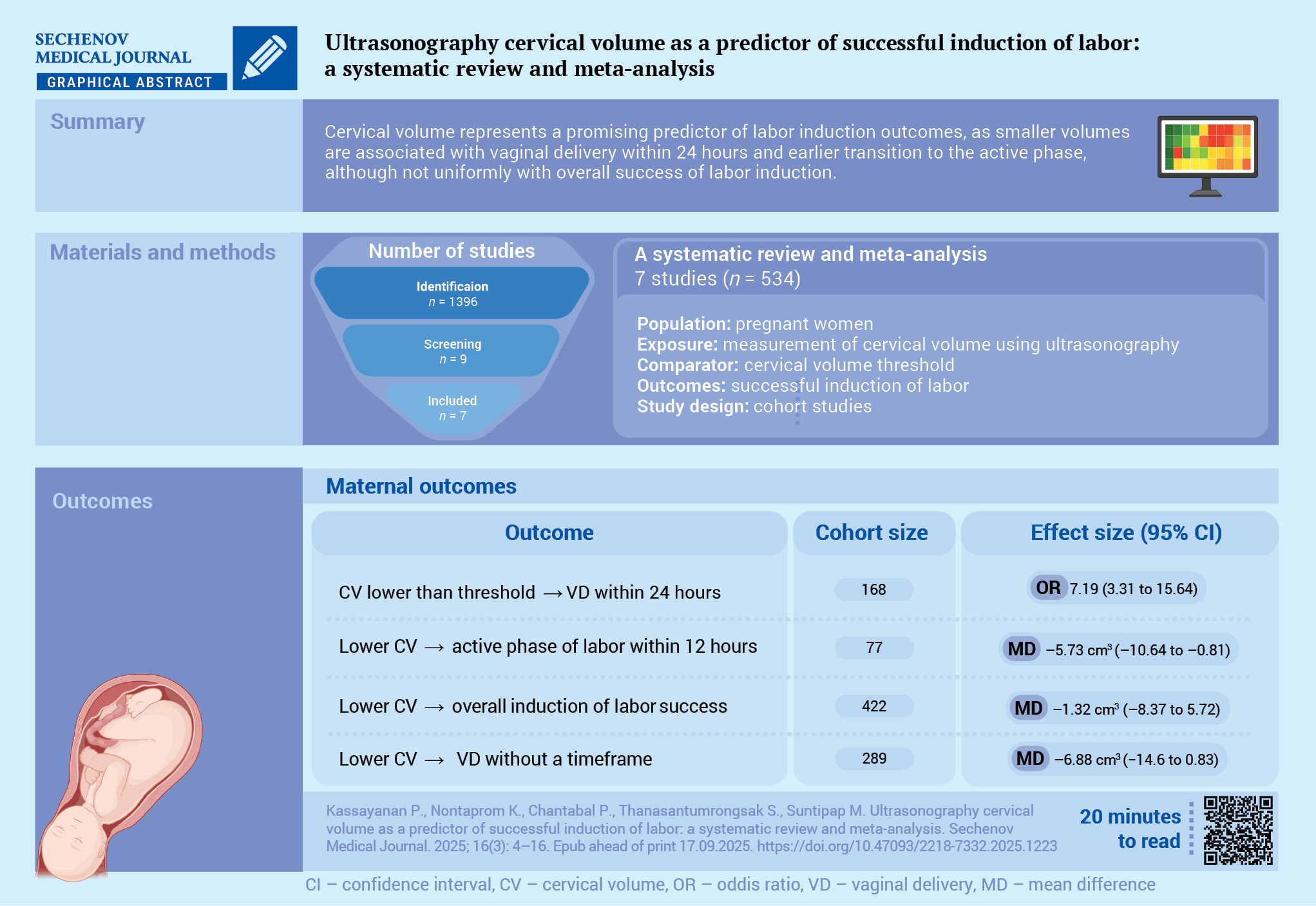
- obstetrics and gynaecology,
- oncology, surgery
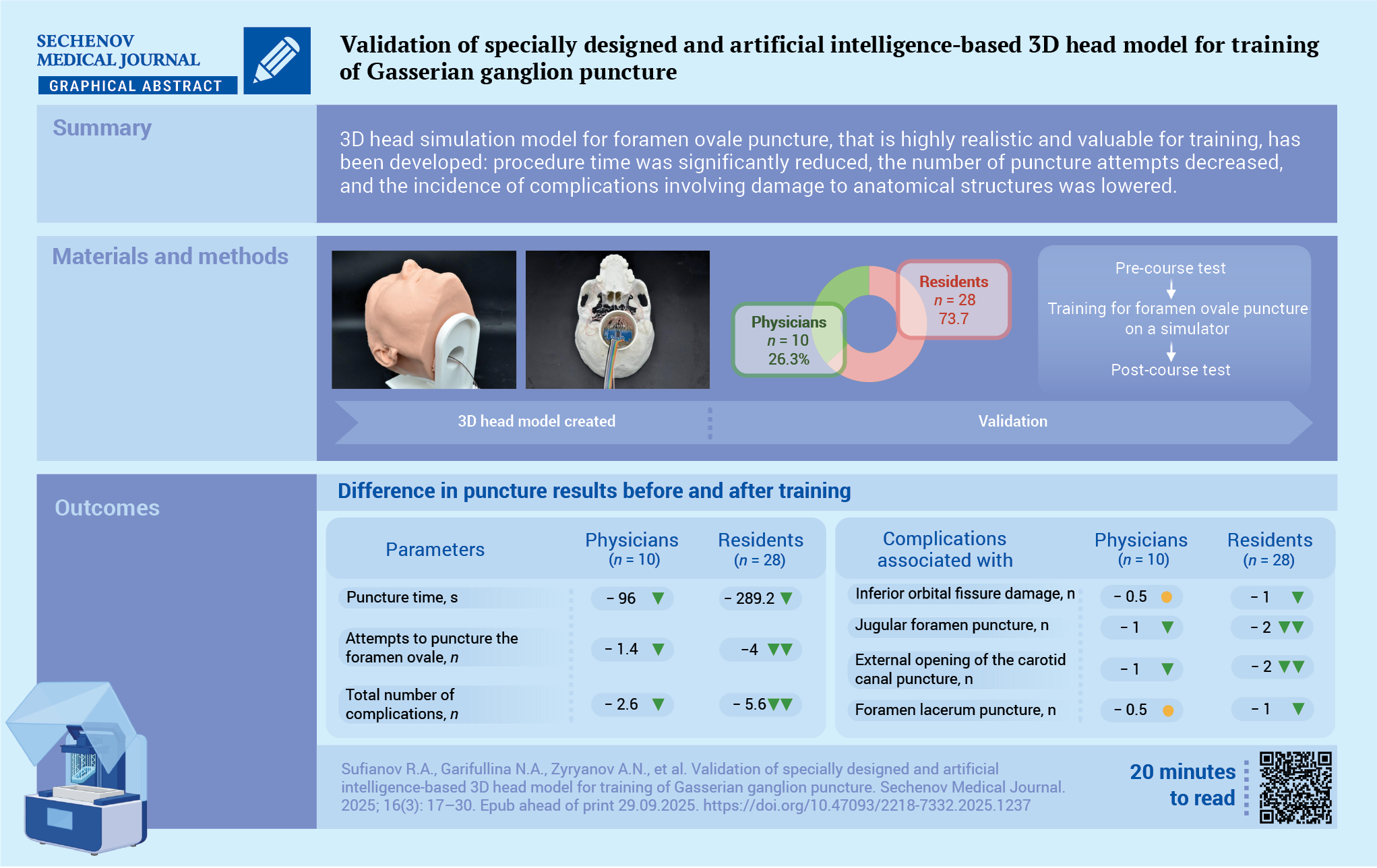
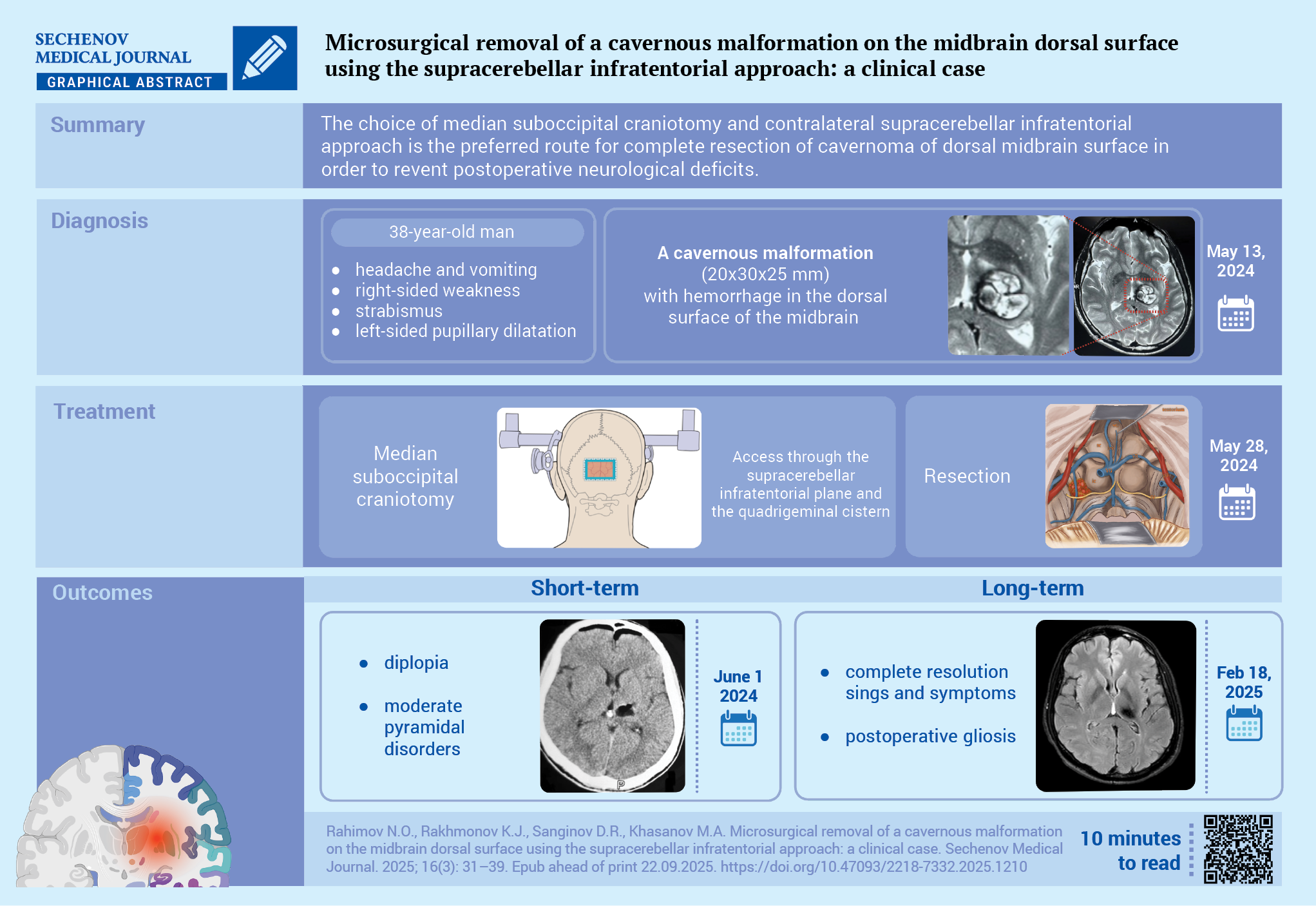
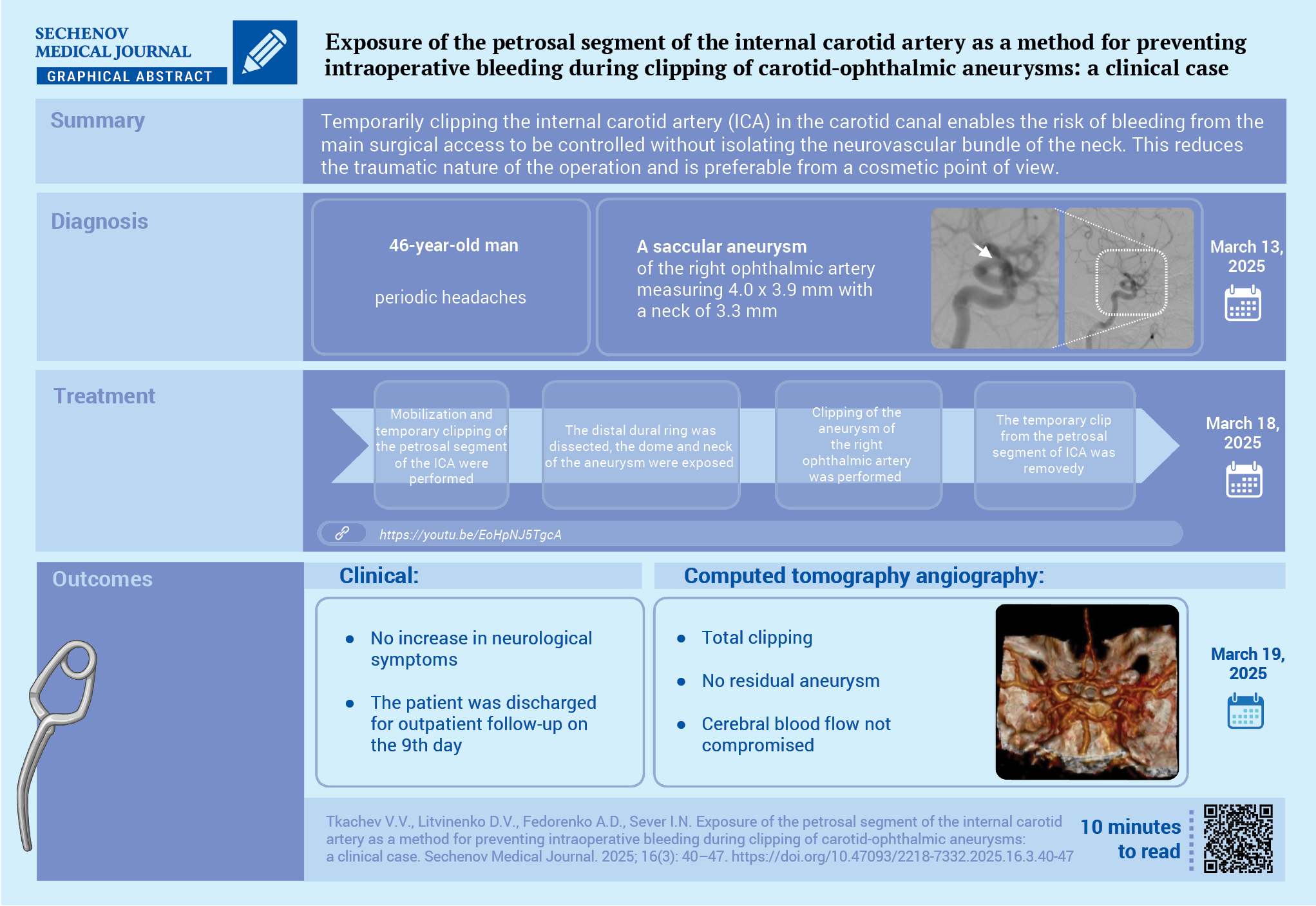
- neurosurgery.
Publication time frames:
5 days - first decision (accept for review or reject the manuscript)
40 days - average duration of the review phase
99 days - from manuscript submission to publication (average)
20% - of all manuscripts submitted during the year were accepted for publication
Mass media state registration certificate PI № ФС77-78884 dated August 28, 2020, issued by the Federal Service for Supervision of Communications, Information Technology and Mass Media (Roskomnadzor).
Current issue
ОBSTETRICS AND GYNECOLOGY
NEUROSURGERY
INTERNAL MEDICINE
Announcements
2026-01-22
Special issue of Neuro-Morphology in the Sechenov Medical Journal
Dear Colleagues,
We are pleased to invite you to participate in a special issue of Neuro-Morphology in the Sechenov Medical Journal by submitting your articles for consideration.
This issue will focus on topics related to the study of the histostructural features of the human nervous system and various animal models.
We will accept manuscripts formatted according to the journal's requirements until June 2026.
Sincerely,
Editors of the special issue:
Sergey L. Kuznetsov,
M.D., Professor and Corresponding Member of the Russian Academy of Sciences; Professor, Department of Human Anatomy and Histology, N. V. Sklifosovsky Institute of Clinical Medicine
Gennady A. Pyavchenko,
M.D., Associate Professor, Department of Human Anatomy and Histology, N. V. Sklifosovsky Institute of Clinical Medicine
| More Announcements... |