NEUROSURGERY 
Aneurysms of the ophthalmic segment of the internal carotid artery (ICA) have traditionally been considered complex, due to the peculiarities of their anatomy, difficult accessibility for open surgery and the risk of deterioration of visual functions. The high variability of the location of carotid-ophthalmic (paraclinoid) aneurysms is the main reason for the lack of a generally recognized clinical and anatomical classification of aneurysms of this localization. In turn, the lack of anatomical unification limits the communication between specialists involved in the diagnosis and treatment of such patients, as well as complicates the comparative analysis of clinical data and the results of microsurgical and intravascular operations. The proposed generalized classification scheme of aneurysms of the ophthalmic segment of the ICA can be used to systematize clinical material, study surgical algorithms in detail and develop optimal treatment tactics for patients with paraclinoid aneurysms.
Machine learning (ML) methodology surpasses the traditional tools of statistical analysis in processing big data clinical datasets .
Aim. To develop an ML algorithm of application of recurrent neural network to analyze clinical datasets of patients with aneurysmal subarachnoid hemorrhage (SAH).
Materials and methods. A big data registry included retrospective data from 2,631 patients with an arterial aneurysm. From these, 390 individuals were selected who required treatment for SAH in an intensive care unit (ICU) setting. The raw dataset contained 7290 features, from which 12 features were selected to train the following ML models: logistic regression, support vector machine, random forest, XGBoost, multilayer perceptron and long short-term memory network (LSTM) were tested. Data preprocessing and modeling were provided in Python (version 3.11.4) using scikitlearn, tensorfl ow, keras and hyperopt libraries. The values and 95% confi dence intervals (CI) of AUROC and AURPC, predictive value, specifi city and sensitivity were calculated.
Results. We recruited 246 (63%) females and 144 (37%) males with mean age of 54±12.9 years. Death occurred in 133 (34%) patients including 33 patients deceased during 24 hours after admission. The best model for predicting lethal outcome was LSTM. After comparison with other ML algorithms LSTM showed the highest predictive values (AUROC – 0.83; 95% CI: 0.72–0.92, AURPC – 0.62; 95% CI 0.39–0.81) in term of in-hospital mortality. For the period in ICU from day 3 to day 6, the model’s positive predictive value was 0.83, sensitivity 0.95 and specifi city 0.58.
Conclusions. LSTM may be applied to development of automatic algorithms in management of critically ill patients after SAH.
One of the ways to improve functional outcomes in patients with ruptured cerebral aneurysms is preventive decompressive craniectomy (DC). Such tactics have not been studied during pregnancy.
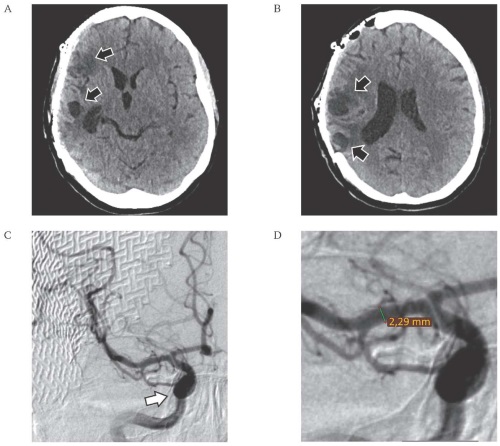
Case report. A 34-year-old female patient, who was 10 weeks pregnant, was hospitalized for an acute headache. According to imaging methods, rupture of the aneurysm of the right internal carotid artery (ICA), subarachnoid parenchymal subdural hemorrhage, pronounced widespread arteriospasm were diagnosed. Consent to surgical treatment with the condition of prolongation of pregnancy was obtained only on the 4th day of the disease against the background of an increase in the volume of subdural hematoma and displacement of median structures. DC was performed and the aneurysm was clipped. The course of the postoperative period was favorable. At 40 weeks of pregnancy, a cesarean section delivery was performed, the child is healthy. Subsequently, cranioplasty of the skull bone defect was performed.
Discussion. The first case of successful treatment of a patient with a ruptured ICA aneurysm in the first trimester of pregnancy using DC is presented. The treatment of pregnant women with ruptured cerebral aneurysms in the first trimester of pregnancy presents significant difficulties in medical, moral, ethical and legal terms. A multidisciplinary approach, a balanced assessment of the severity of the disease and pregnancy, individual risks of surgery and potential complications, the volume of diagnostic procedures and intensive care measures performed, make it possible to preserve the life and health of the mother and fetus.
In large internal carotid artery (ICA) aneurysms, the angle of the mandible becomes an anatomical obstacle to creating an adequate access. Widening the access can be achieved by performing a mandibular osteotomy.
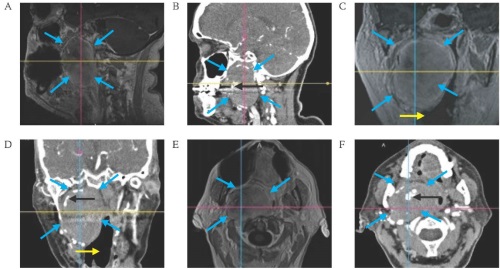
Case report. A 70-year-old female patient was admitted to hospital with complaints of hoarseness of voice, dyspnoea and congestion of the right ear. Objective examination revealed nasal respiratory distress due to nasopharyngeal compression by a voluminous mass, mild dysarthria, dysphonia, tongue deviation to the right, paresis of the right soft palate and right vocal cord. Computed tomography and magnetic resonance imaging showed a 50×49×60 mm thrombosed ICA aneurysm in the carotid space. Surgical management was performed by a multidisciplinary team including neurosurgeons, otolaryngologists and maxillofacial surgeons. Extended access was achieved by intraoral mandibular osteotomy followed by mobilization. Early postoperative resolution of neurological symptoms was observed.
Discussion. To gain access to giant aneurysms of the cervical branch of the ICA, it is possible to use the technique of intraoral osteotomy of the mandible. This reduces trauma and the risk of complications, while increasing the radicality of the main stage.
Intradural herniation of the intervertebral disc (IHID) is extremely rare. There are only a few reports of cranial migration of an intradural fragment of a sequestered disc herniation.
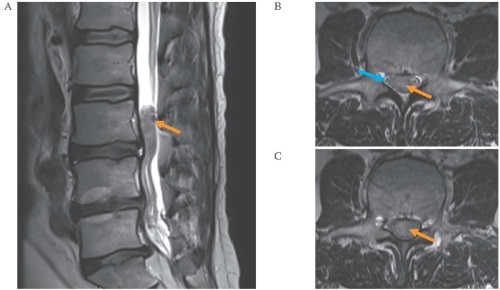
Clinical case. A 51-year-old patient who had previously undergone two operations at L5–S1 and L4–L5 levels was admitted to the hospital with complaints of low back pain with radiation to both legs, numbness in the perineum and inner surface of the thighs, urinary retention, constipation. Magnetic resonance imaging revealed a 30 mm mass located at the level of the L3 vertebral body, within the dural sac and filling its entire transverse diameter. The cauda equina nerve roots were compressed. Surgery was performed: the herniated sequestrum (30×10×10 mm) was separated from the nerve roots fixed to it and removed. After surgery, sensation in the buttocks and inner thighs returned, and urinary urge appeared. Rehabilitation is ongoing.
Discussion. In most cases, IHID is diagnosed intraoperatively. In the presented case, the genesis of the formation remained unclear before surgery, so a laminectomy approach was chosen, which allowed for extensive revision of the intradural space, thorough radiculolysis, and identification of the cranial migration of the sequestrated disc herniation. The only effective treatment for IHID is surgery.
EDITORIAL 
ISSN 2658-3348 (Online)